Hello, I'm Big Research
I’m the thing that means Big Breakthroughs can be made so the health of little lives is improved.
Big Research is done by people who notice, ask lots of questions, and have clever ideas. It can involve a lot of different people, and it can take a lot of time. It takes a lot of heart and a lot of brain power. It also takes a lot of money.
And that is what Cure Kids helps with. To raise the money for the hearts and brains to do the big research to improve little lives.
We fund research to...
-
Understand the cause
We fund researchers to find out what causes the diseases and health conditions that affect Kiwi kids, so that we can discover new ways to prevent, treat, and cure disease.3 active Cause projects -
Improve the care
We fund researchers to improve the standard of care for Kiwi kids who live with serious health issues, by finding creative ways to reduce pain, extend life, or improve the quality of life for children.27 active Care projects -
Discover the cure
We fund researchers to develop innovative devices, medicines, or methods which have the potential to prevent or cure childhood illnesses.4 active Cure projects
Big Research
We are currently supporting over $10 million of child health research projects.
Learn more-
Preterm Health
4 Active projects$464.8K -
Childhood Cancers
2 Active projects$3.2M -
Maternal and Infant Conditions
4 Active projects$751.4K -
Rheumatic Heart Disease
6 Active projects$2.8M -
Childhood Development and Learning Difficulties
2 Active projects$228K -
Neurological and Neurodevelopmental Disorders
3 Active projects$749.2K -
Endocrinology, Metabolism & Nutrition
1 Active project$125K -
Mental Health and Wellbeing
8 Active projects$1.2M -
Genetic Conditions and Rare Disorders
3 Active projects$801K -
Respiratory Conditions
5 Active projects$862.6K -
Infectious Disease
2 Active projects$219.7K -
Gastrointestinal Conditions
1 Active project$600K
A series of studies on risk factors for sudden unexpected deaths in infancy (SUDI), leading to advice that has prevented at least 200 deaths every year (and many more around the world)
A Maternal and Infant Conditions project
Improving the remote care of children with hydrocephalus (a dangerous and abnormal buildup of fluid in the brain) via a tiny brain implant monitor
A Neurological and Neurodevelopmental Disorders project
Discovering a potential treatment for a terrible neurodegenerative condition called Batten disease
A Genetic Conditions and Rare Disorders project
Identifying a safer test to prevent eye disease in premature babies
A Preterm Health project
Discovering some of the genes which cause epilepsy in children, allowing for more accurate diagnosis and better treatments for children, parents, and their families
A Neurological and Neurodevelopmental Disorders project
Our research in action
We improve health and wellbeing for tamariki Māori
We’ve got a unique population here in NZ, and Māori children have a genetic heritage found nowhere else in the world.
To enable health and wellbeing for tamariki Māori, we need to use local knowledge to design homegrown solutions to tackle NZ-specific health problems.
Cure Kids is proud to work alongside Māori health experts so we can be sure we’re allocating funds and support to the very best projects.
The Advisors
Behind every funding decision we make is a panel of advisors – a talented bunch of 10 who together make up Cure Kids Medical and Scientific Advisory Committee.

Professor Stephen Robertson
Professor Stephen Robertson has been the Cure Kids Chair of Paediatric Genetics at the University of Otago since 2002.
Prof Robertson has gained international acclaim in his field for his expertise in the field of genetic mutations, specifically those affecting the skeleton and the brain.
He completed his undergraduate degree at the University of Otago, Dunedin, where he would eventually return more than a decade later. During his absence from Otago, he held the prestigious Nuffield Scholarship at the Institute of Molecular Medicine at the world-leading Oxford University. Also specialising in paediatrics, Prof Robertson is a clinician who sees children with varying degrees of malformation on a regular basis.
Prof Robertson’s work has seen him and his team discover genes that are implicated in a number of genetic disorders. These include familial disorders where a number of members of a particular family are affected with life-affecting, even fatal, conditions. One such story involved Robertson working tirelessly with a whanau in the far North who were inexplicably losing children soon after birth. After a long journey, he identified the gene which was responsible for the babies’ deaths enabling a diagnosis to be made. This was also fundamental in giving the whanau information regarding future offspring as well as the peace of mind of knowing what happened to their loved ones.
“What we’re about is helping people understand and live with disability as best they can, and part of that’s through giving information about what causes it.”
Prof Robertson and his team continue to work to characterise and better understand rare, yet significant, diseases that affect a number of New Zealand children.

Dr Patricia Anderson
Dr Anderson is a trained nurse, with a MPhil in clinical pharmacology and a PhD in medicine and therapeutics. Her previous research interests included pharmacogenetics, insulin resistance and the metabolic syndrome. She previously spent a decade researching and lecturing in clinical pharmacology and statistics at universities in Hong Kong and working in the region’s Poisons Information Bureau.

Professor Andrew Day
Professor Andrew Day holds the chair of Paediatric Research at University of Otago, Christchurch.
Professor Andrew Day undertook his medical training at University of Otago, New Zealand. After his initial paediatric training in Christchurch, he completed clinical and research fellowship training at the Hospital for Sick Children, Toronto, Canada. In 2000, he took up appointments at the University of New South Wales and Sydney Children’s Hospital in Sydney, Australia. Professor Day then returned to NZ in 2009 to take an academic position at University of Otago (Christchurch) and a clinical position (Paediatric Gastroenterologist) at Christchurch Hospital. In 2017, Prof Day was appointed as Cure Kids Chair of Paediatric Research in Christchurch.
The overall objectives of Prof Day’s ongoing research activities are to delineate and define aspects of gastrointestinal inflammation, especially in the context of inflammatory bowel disease, and to define how interactions occurring at the gastrointestinal epithelial border between the host and the environment affect disease pathogenesis and manifestations. This has focused especially upon epithelial responses to inflammatory stimuli, host innate immune responses and to modulation of these responses with therapeutic intervention, providing clinical relevance to laboratory activities. He has an ongoing active and productive research program, with local and international collaborations, leading to more than 220 peer-reviewed publications and numerous other presentations or publications.

Professor Stuart Dalziel
Professor Dalziel is the Cure Kids Chair of Child Health Research.
He is a Professor in the School of Medicine’s Departments of Surgery and Paediatrics, Director of Emergency Medicine Research and a Paediatric Emergency Medicine Specialist, Children’s Emergency Department, at Starship Children’s Hospital. He is also the current chair of the Paediatric Research in Emergency Departments International Collaborative (PREDICT, Australasia’s paediatric emergency medicine research network) and Vice-Chair of the Paediatric Emergency Research Network (PERN), a collaboration of the six major international paediatric emergency medicine research networks.
Originally from Hawke’s Bay, he trained at the Universities of Otago and Auckland, returning to New Zealand over a decade ago following a fellowship post at Great Ormond Street Hospital for Children in London. Professor Dalziel’s research is strongly aligned to his everyday clinical practice as a Paediatric Emergency Medicine Specialist. It focuses on both medical emergencies, such as status epilepticus (the most common paediatric neurological emergency), and common paediatric conditions, such as asthma and bronchiolitis (the most common reason for infants to be admitted to hospital). Professor Dalziel has received numerous local and international awards for mentoring and research excellence. He is actively involved in the leadership of a number of international research networks which directly address important questions related to the acute care of children.

Professor Terryann Clark
Her specialist expertise is in mental health, nursing, social determinants of health, and health services for young Māori. Much of her research has focused on depression, suicide, and delivery of equity in mental health for young Māori. Prof Clark also holds a range of governance and advisory roles related to young people, Māori health, and mental health. Since 1998 Prof Clark has been the Principal Investigator and Co-Lead of the Youth2000 series of national surveys on youth health and wellbeing. She is a founding member of the national Adolescent Health Research Group. In 2022, Prof Clark joined Cure Kids' Medical & Scientific Advisory Committee.

Associate Professor Chris McKinlay
Dr Chris McKinlay received his medical education at the University of Auckland, before specialising in paediatrics and neonatology in Auckland and Melbourne. He was awarded a PhD in Paediatrics from the University of Auckland in 2012. He is an Associate Professor in the Department of Paediatrics: Child and Youth Health and works as a consultant neonatologist at Middlemore Hospital. His research focuses on the early life origins of metabolic disease, lung disease and developmental impairment. He undertakes clinical trials to improve the care of newborn babies, ultimately aiming to improve their long-term health.

Professor Esko Wiltshire
Professor Wiltshire completed his undergraduate training in Medicine at the University of Otago, before working in the greater Wellington region while completing a Diploma in Obstetrics and Gynaecology and Diploma in Paediatrics. He undertook advanced training in general paediatrics, followed by paediatric endocrinology and metabolic disease, in Adelaide, South Australia. During this time he also completed his doctorate, investigating early vascular disease in children with diabetes, before returning to Wellington as a senior lecturer in the Department of Paediatrics and Child Health, University of Otago Wellington and Paediatrician/Paediatric Endocrinologist for CCDHB. He has overseen development of services in Paediatric endocrinology and diabetes since 2001.
Professor Wiltshire's primary areas of research involve investigation of the acute and chronic complications of diabetes, particularly their pathophysiology and early development, and treatment. The aims of this research are to identify factors involved in the early pathogenesis of the vascular complications of diabetes, when interventions will have the greatest effect along with identification and treatment of hypoglycaemia. More recent research has been investigating use of technology in both type 1 and type 2 diabetes. he is also involved in clinical research in a range of other endocrine conditions. He has served as a council member and president of the Australasian Paediatric Endocrinology Society and was past chair of the International Consortium for Paediatric Endocrinology (an organisation linking all the Paediatric Endocrine Societies around the world).

Professor Te Kani Kingi
His specialist expertise is in mental health, psychometrics, health services, and Māori health. Prof Kingi leads a research theme for the 'Growing Up in NZ' longitudinal study of child health, and holds a range of governance roles throughout the health, research, and science sectors, including for the Royal Society of NZ, the Health Research Council, EMERGE Aotearoa, and the National Institute for Economic and Demographic Research. Prof Kingi is on Cure Kids' Medical & Scientific Advisory Committee, and leads the process for peer review of Grant applications by Māori experts.

Associate Professor Teuila Percival
She has specific expertise in respiratory and rheumatic heart disease in young children, and her research has encompassed maternal and child health, climate change and health, child obesity, health systems and informatics.
Assoc. Prof Percival has worked in both New Zealand and throughout the Pacific region in both clinical and research roles.
She is Vice-President of the Pasifika Medical Association, Chair of Fale Futures Trust, Chair of South Seas Healthcare, a trustee of Ta Pasifika Primary Health Organisation, and serves on a number of government health advisory groups. Assoc. Prof Percival was awarded a Queen’s Service Order medal in 2010, and in 2023, she received a King's Birthday Honours as Dame Companion of the New Zealand Order of Merit for services to health and the Pacific community.

Professor Tony Walls
Prof Walls graduated from the University of Otago and trained as a general paediatrician. He then moved to London to train in Infectious Diseases at the Royal London Hospital and Great Ormond Street Hospital. Before returning to New Zealand he worked as a Consultant in Paediatric Infectious Diseases at the Sydney Children’s Hospital, where he was the lead clinician for the Paediatric HIV Service.
His current research interests include the epidemiology of infections in children, the diagnosis and management of paediatric bone and joint infections and vaccinating pregnant women to protect their infants. He is Co-Director of the recently established Research for Children Aotearoa research collaborative which brings together researchers from across institutions, regions and disciplines to enhance community-led child health research.
Professor Walls is also an advisor to PHARMAC and the New Zealand Ministry of Health on vaccine policy matters, and is an author on the National Immunisation Handbook.
Our research in action
95 active projects, 106 phenomenal researchers
-
Dr Jason Turuwhenua
-
Dr Fiona Langridge
-
Emeritus Professor Sally Merry
-
Professor Lynette Sadleir
-
Professor Jane Harding
-
Professor Cameron Grant
-
Dr Christine McIntosh
-
Professor Peter Gluckman
-
Dr Simerdeep Dhillon
-
Professor Barry Taylor
-
Dr Manisha Sharma
-
Emeritus Professor Ed Mitchell
-
Dr Dianne Sika-Paotonu
-
Dr Rachel Brown
-
Professor Esko Wiltshire
-
Assoc Prof Kaaren Mathias
-
Professor Trecia Wouldes
-
Professor Russell Snell
-
Dr Samantha Marsh
-
Professor Rod Dunbar
-
Dr Rebecca Findlay
-
Associate Professor Nikki Moreland
-
Dr Hilary Sheppard
-
Dr Guido Wassink
-
Dr Nadia Mitchell
-
Professor Simon Malpas
-
Dr Jennifer Hollywood
-
Professor David Fergusson
-
Associate Professor Siouxsie Wiles
-
Professor Lianne Woodward
-
Professor Greg O'Grady
-
Dr Jiney Jose
-
Dr Mark Oliver
-
Dr Lisa Pilkington
-
Professor Leonie Pihama
-
Prof Massimo Caputo
-
Dr Angus Lindsay
-
Professor Frank Bloomfield
-
Distinguished Professor Linda Smith
-
Emeritus Professor Keith Grimwood
-
Associate Professor Mhoyra Fraser
-
Dr Nicola Ludin
-
Dr Tania Cargo
-
Professor Stephen Robertson
-
Associate Professor Jo James
-
Dr Rosie Dobson
-
Dr Ben Albert
-
Associate Professor Nigel Wilson
-
Dr Mariana Muelbert
-
Professor Boyd Swinburn
-
Dr Jacelyn Loh
-
Professor Barbara Galland
-
Professor Ian Morison
-
Associate Professor Chris McKinlay
-
Dr Tanya Cully
-
Dr Jennifer Knopp
-
Associate Professor Ehsan Vaghefi
-
Associate Professor John Thompson
-
Mrs Nicky-Marie Kohere-Smiler
-
Dr Sarah Fortune
-
Associate Professor Sarah Hetrick
-
Distinguished Professor Margaret Brimble
-
Professor Andrew Day
-
Dr Amy Scott-Thomas
-
Dr Emily Perelini
-
Professor Rich Masters
-
Associate Professor Max Berry
-
Dr Patricia Anderson
-
Associate Professor Alys Clark
-
Dr Nicholas Bowden
-
Dr Teresa Gontijo de Castro
-
Ass Prof Laurie McLay
-
Associate Professor Martin De Bock
-
Professor Peter Vuillermin
-
Dr Andrew Wood
-
Associate Professor Andrew McDaid
-
Dr Yvonne Anderson
-
Sir Bob Elliott
-
Dr Shirley Tonkin
-
Associate Professor David Reith
-
Dr Anneka Anderson
-
Dr Jonathan Skinner
-
Associate Professor Catherine Byrnes
-
Dr Julie Bennett
-
Dr Mairin Taylor
-
Dr Joanne Choi
-
Emeritus Professor Lesley McCowan
-
Associate Professor Teuila Percival
-
Dr Seini Taufa
-
Dr Amber Young
-
Professor Tony Kettle
-
Associate Professor Laurens Manning
-
Dr Peter Choi
-
Professor Te Kani Kingi
-
Dr Louise Bicknell
-
Professor Terryann Clark
-
Professor Tony Walls
-
Professor Nick Draper
-
Assoc Prof Justin Dean
-
Professor Diana Lennon
-
Professor Stuart Dalziel
-
Professor John Everatt
-
Associate Professor Simon Swift
-
Dr Alison Leversha
-
Dr Alexandra Wallace
-
Professor David Barker
-
Associate Professor M. FraserExosome-based diagnostics: A Better Start For Baby’s BrainAwarded $109,763Preterm Health
-
Professor A. DayDiet and IBD: New approachesAwarded $600,000Gastrointestinal Conditions
-
Prof M. CaputoImproving outcomes of aortic valve replacement in children and young adults with rheumatic heart diseaseAwarded $124,239Rheumatic Heart Disease
-
Assoc Prof J. DeanMitochondrial dysfunction and delayed treatment of preterm brain dysmaturationAwarded $124,534Preterm Health
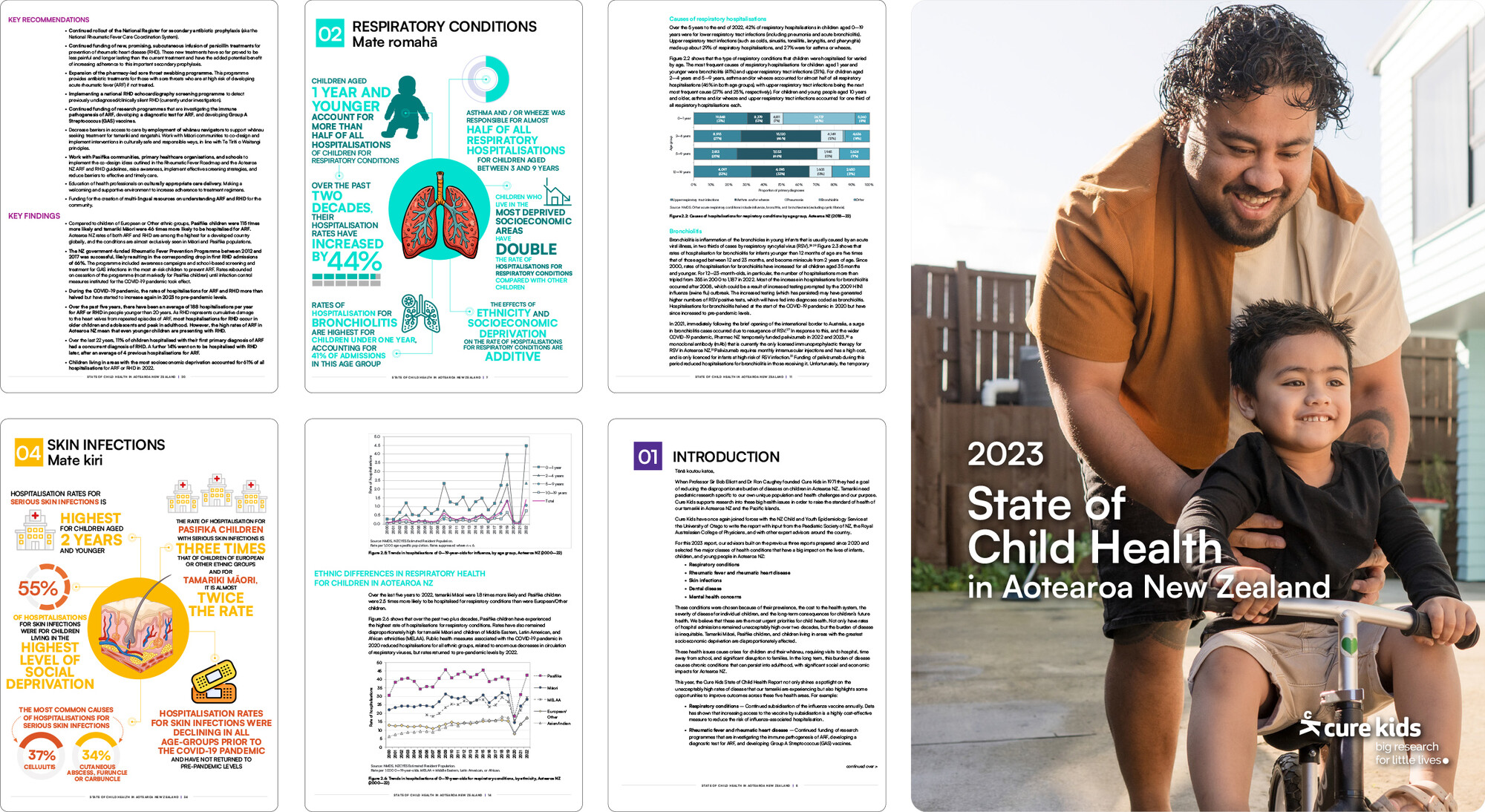
2021 Report
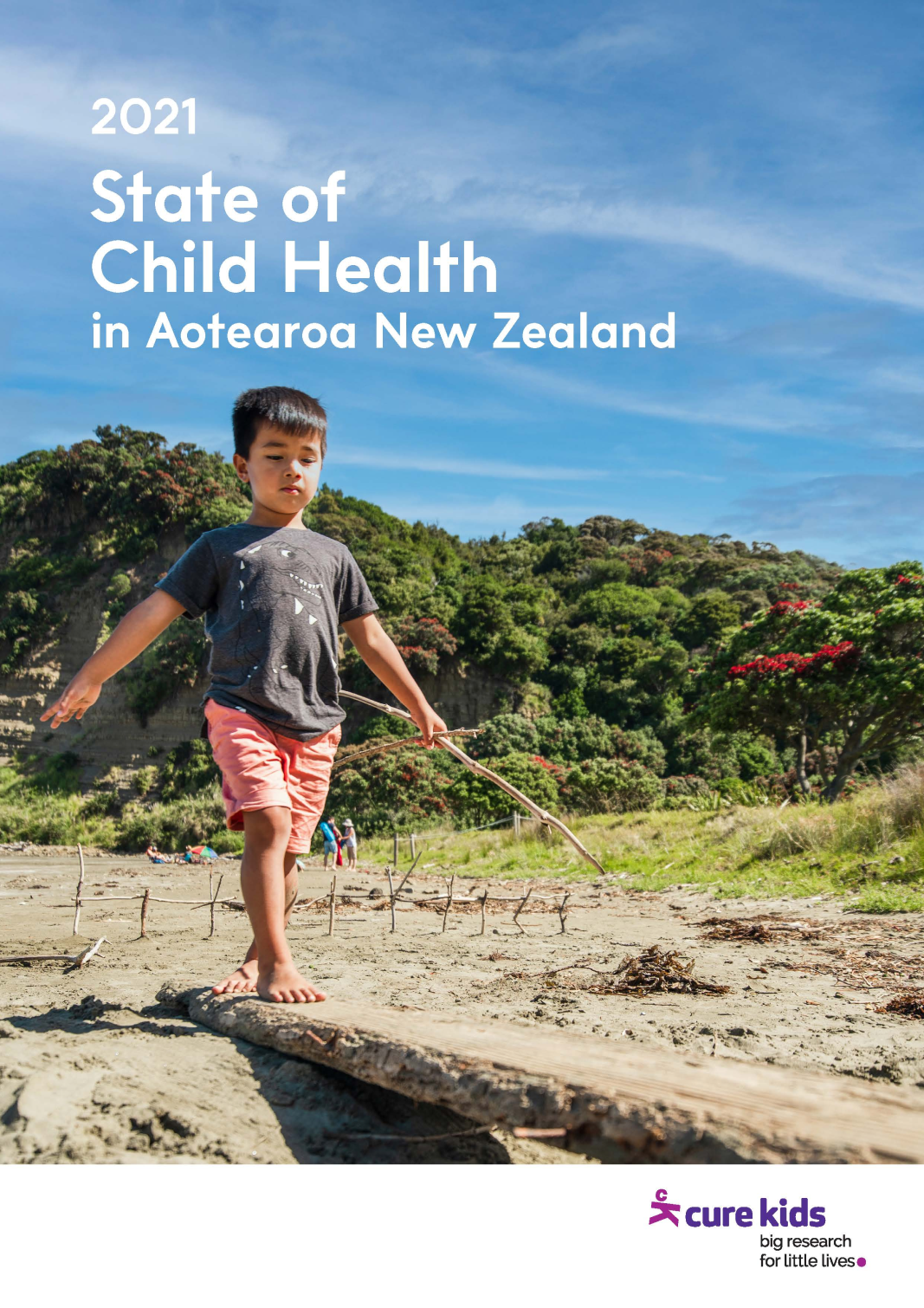
State of Child Health in Aotearoa New Zealand
Cure Kids' inaugural State of Child Health Report 2021 sets out three key indicators to benchmark the health of New Zealand children.